Burnt out junior doctors face working conditions that put their lives at risk and are leading to a brain drain of talent from the state, they claim as negotiations over better pay and hours continue with the government.
Talks between NSW Health and the Australian Salaried Medical Officer’s Federation (ASMOF) have so far failed to reach a resolution, with the Industrial Relations Commission ordering doctors refrain from industrial action for three months.
The doctors’ strike a fortnight ago was the first in 25 years, with public sector doctors of varying experience and specialty calling on the Minns’ government to address onerous working conditions and pay.
“Doctors all over NSW health are tired, burnt out, and numb,” said junior medical officer (JMO) Dr Serina Dabous. “It’s hard to go to work knowing your colleagues a one-hour flight away are well supported, well paid and mostly enjoy going to work.”
Intern junior doctors, or first year JMOs, face the brunt of poor conditions in NSW, according to health workers. In NSW, a junior doctor makes about $38 an hour in their first year, however in Queensland, the same position is paid $45 an hour.

Dr Dabous, who moved back to NSW after studying in Queensland, said the working conditions had led to a brain drain of doctors from the state.
“There hasn’t been a single day in the last 10 weeks where I don’t question and often regret my choice of moving back to NSW health instead of staying in Queensland Health,” she said.
“JMOs in NSW are poorly paid for the sheer volume of work we are doing. The conditions in many instances are extremely unsafe. Going from being a medical student in a different state to now taking care of over 40 patients at once, without even having time to get used to the system, was difficult. I broke down three times in my first week.
My mental health is the worst it’s ever been. I haven’t been able to properly take care of myself mentally or physically. My life revolves around work and my patients.
“For my friends who are interning in Queensland, it is a different picture. They finish on time; they get paid more. They enjoy going into work. They have social lives. They are happy.
“I moved for my family. But at what cost? My mental health is the worst it’s ever been. I haven’t been able to properly take care of myself mentally or physically. My life revolves around work and my patients.”

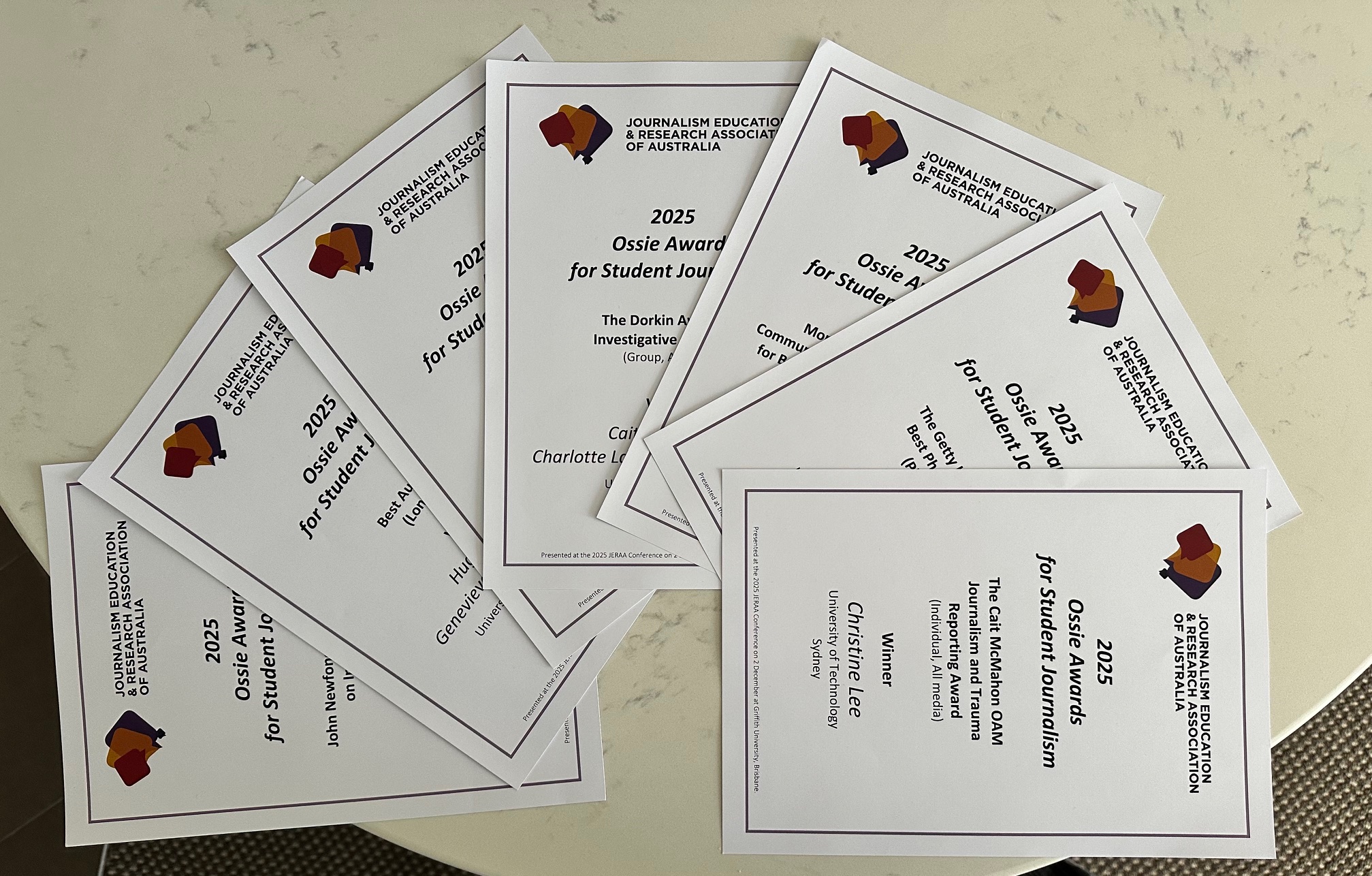
Dr Dabous graduating last year. Supplied.
Although NSW and Victoria have a comparable number of doctors, those in Victoria earn more than their counterparts in NSW, a fact NSW Health Minister Ryan Park claimed was due to wage suppression by the previous government. The NSW government is offering doctors a 10.5 per cent pay rise over three years.
However, Dr Joel Riley, a rheumatologist in Dubbo who participated in the strike, said the wage offer would not ensure parity with other Australian states nor factored in inflation. Subsequently, he added, it would become difficult to recruit doctors in the public sector.
“They acknowledge there has been a wage reduction, yet why does their proposed solution do absolutely nothing?” Dr Riley asked.
“I could quit my job tomorrow and make an extra $200 000.”

Alongside pay concerns, many doctors have claimed the strike was largely driven by unsafe working conditions.
“Our junior doctors have minimal restrictions on their safe work hours,” said Dr Riley. “I remember when I was a junior doctor they would roster us for six nights in a row.
“They wouldn’t roster us for seven nights because otherwise they [legally] would have to give us a week off.”
On my way home from work, I actually have a set area on my route where I go and sleep in front of a steel factory just so I don’t die on my way.
Dr Fahad Khan, a junior doctor in Western Sydney, said he had to pull over and take a nap on his way home from work each night in case he fell asleep at the wheel.
Dr Kahn, who has documented his experiences in becoming a doctor to his nearly 400,000 TikTok followers, posted: “You can call this a pay dispute all you want, but the moment a doctor dies on the road because they fell asleep at the wheel, you can give them as much pay as you want- but it is no good if the doctor is dead.
“On my way home from work, I actually have a set area on my route where I go and sleep in front of a steel factory just so I don’t die on my way.”
@fahad_teaches Shame on you Ryan Parks and Chris Minns. #doctorstrike #doctor #australia
Dr Dabous added: “I got into a car accident on my second day as a junior doctor and wrote off my car. Whiplash and all.”
While Dr Riley said: “The conditions of work need to be changed; they need to be made safe. I lost a friend during my internship to a car accident.”
They all said working conditions are yet to be addressed by the NSW government.
Doctors in both Dubbo and Orange also participated in the strikes, calling for better conditions. Among them was Dr Riley, the only rheumatologist in his district.
In rural areas, issues regarding pay and working conditions significantly impact the existing limited access to care.
“I see patients that once had a fixable problem, but it wasn’t fixed in time because there is a lack of access to care,” said Dr Riley.
“People turn up with life-threatening thyroid disease. This should not happen in a first world country.”
Statistics from the Australian Institute of Health and Welfare affirm this, showing that people in remote and very remote areas are hospitalised for preventable conditions at rates two to three times higher than those in urban areas.

Doctors say without greater investment in public healthcare, it is also becoming increasingly difficult to hire doctors in rural areas.
“Last year we had no domestic applicants,” Dr Riley said.
“I don’t know how you can look at healthcare, particularly rural healthcare in this state and think it deserves this.
“What happens in these circumstances is that I only get to see the worst of the worst cases. I am burnt out.”
Without guaranteed changes for NSW doctors, many fear NSW Health may face a crisis like the United Kingdom’s NHS.
As a medical student who did a portion of her studies in Scotland, Noor Ibrahim has first-hand experiences in the NHS.
“After seven years of medical school, which have been really tough, to see these working conditions and such a poor pay that doesn’t reflect the nature of the work we do, it is a slap in the face,” she said.
“I think the general public needs to be worried about this, because we are all exposed to hospitals at one point in our lives. Our loved ones will be exposed to hospitals. It is not just a junior doctor problem.”